26 August 2020
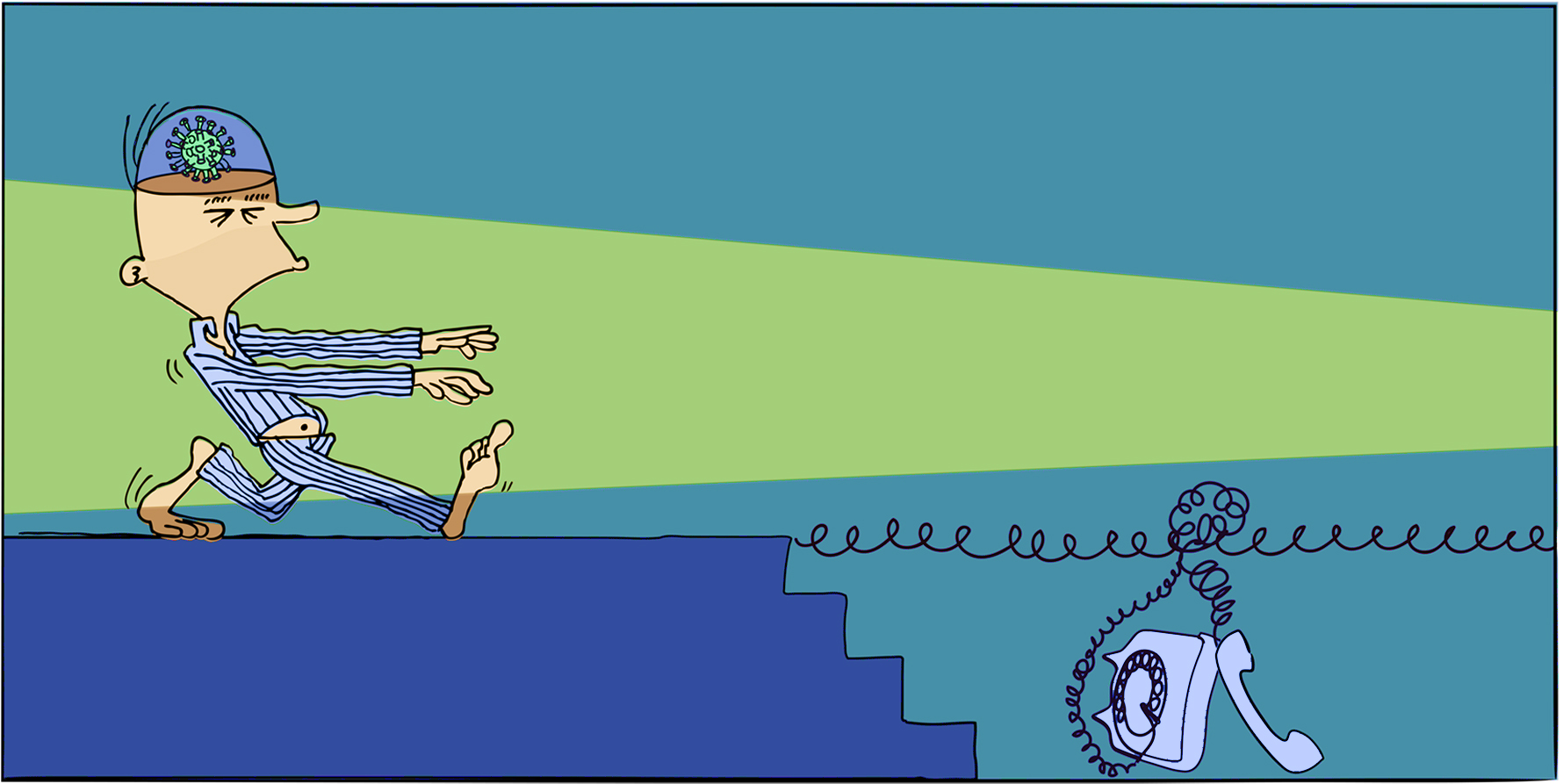
Are we idiots sleepwalking through a crisis? Or can we learn and adapt?
In Tuesday’s COVID digital pivot threats and opportunities webinar the normally eloquent and politic Medical Software Industry Association of Australia (MSIA) CEO Emma Hossack used Checkov’s quote to underline the difficulties we likely will end up facing as COVID winds down and we try to bottle the processes behind some of the amazing collaborative efforts that have taken place in healthcare to solve big issues during the crisis.
“…did Emma Hossack just refer to everyone in the system (albeit tangentially) as an idiot?” I scribbled into my notebook.
But before I could stop to consider the implications, a similar observation was made by the CEO of the Australian Digital Health Agency (ADHA), Bettina McMahon. She said, “we need to be careful we don’t sleepwalk out of this crisis…”, implying, again somewht tangentially, that we may have been “sleepwalking in the crisis”.
Sleep-walking idiots then?
Of course, neither Hossack nor McMahon were meaning in any way to denigrate the amazing efforts of collaboration that have taken place between government, doctors and industry during COVID-19. Some of the successes have been spectacular, and well publicised. And they both expressed excitement and admiration over what has been achieved during COVID-19 by the sector.
But they are wondering how the digital health sector and government might manage to codify how so much innovation could be achieved in such a short amount of time, in order lock in some of the progress and fundamentally shift the healthcare innovation paradigm, or lack thereof, we’ve been stuck in for the past couple of decades. Once out of this crisis, will much of what we are seeing in terms of stunning progress slow and stop, and the rest of what’s left over drift back to the ‘bad old days’.
‘Bad old days’ might be a strange way to think about pre-COVID days, but from a health system innovation perspective, COVID induced system innovation is one silver lining we cling too with some hope.

When asked if the COVID crisis was enough to shock the Australian digital health scene out of its slumber “for ever” Grahame Grieve, the founder of global health interoperability resource and standard, FHIR, said “probably not”. He said that the situation in Victoria nearly pushed us to that extreme but that, “thank heavens”, the situation looks like it has been brought under control.
Like McMahon and Hossack, Grieve has been enthused somewhat and even energised by what has been achieved in the crisis. But he sees a lot of complexity between management in a crisis and out of it.
On his website Grieve outlines one of the fundamentals of communication and interoperability in health like this:
“If you want two IT systems to interchange data successfully, you’ve got to get alignment between the people who write them, manage them, and use them. The technical challenges the system maintainers face when making changes are miniscule compared to the problem of getting the various people to agree with each other.”
In yesterday’s webinar Grieve made reference to this same issue by saying “we should not say ‘herding cats’, we should say herding people, because herding people is much harder and that’s what we are trying to do here”.
Herein seems to lie the major issue for bottling the secret sauce that we’ve been pouring over aspects of the health sector for the past few months to help manage COVID-19.
Technology was never the problem. Nor even the idea of ‘interoperability’. It is the willingness and ability of people to collaborate and co-operate.
Remember, key individuals might be willing, but stuck in a government department, agency or a company where such co-operation is simply not feasible on a day to day basis.
But in a crisis? What might normally be seen as rash, even dismissable, behaviour, can be forgiven in the name of the greater immediate good.
All over the world you can attend webinars on COVID-19 induced innovation. It’s a hot topic creating a lot of excitement.
eHealth NSW CEO, Dr Zoran Bolevich, said of the phenomena recently that
“There’s opportunity for health systems to leverage from this crisis both abroad and in Australia to pick up some significant learnings, such as the ethos of agility and working together across traditional boundaries, both professional and governmental and engaging industry in a novel way.”
The question some of our key healthcare change agents are increasingly asking is, how exactly?
Or, perhaps even more pragmatically, who?
If you ask ‘who’ has the power, influence and the ability to adopt and institutionalise some significant learnings COVID-19 has driven us too, the banal technical answer to the question is Dr Brendan Murphy (Secretary of Health), closely followed by Greg Hunt (our Federal health minister) with Scott Morrison (our PM) in secure and cheer leading tow.
If we look at this way, at least we are down to dealing with people and not the technology so much.
Unfortunately, there are lot of people to herd before these three even appear in the picture.
Getting these three aligned in any way for anything in the country is the job of an army industry and sector lobbyists from all walks.
Although healthcare is our biggest government spend, it’s never been seen by government as our biggest problem. So it has always been out-lobbied for attention by more visible, well funded and sexy lobby groups, such as the big end of town miners.
But then COVID-19 arrived, and health definitively became all our biggest problem.
While it’s all our biggest problem we have a window to figure out the question being asked by McMahon and Hossack. How do we capture the change dynamic that COVID has created and keep deploying it moving forward?
Says Grieve, “we’ve certainly got a serious challenge in front of us around the way that we develop community agreement about how things should be done.
“Sometimes it’s called standards. Sometimes we loosely call it, our vendors and governments collaborating. And sometimes it gets other names.
“I have to hope that we as a community can get together behind this and get a working process. But no single party can just magically make a working process happen. “
So, no “magic” to be had here?
Hossack points out that there has never been a time when communication between the government and vendors has been better, and when both have reasonably well aligned objectives. She thinks that is likely to convert in one way or another into an improved innovation ecosystem for health moving forward.
“It is the first time you’re getting someone very high in the department [of Health] saying we really want to hear from you because we don’t know what we don’t know,” she said in relation to vendors talking with government about the crisis.
“That was incredibly pleasing for industry. We were able to put together a whole lot of really clean, sharp responses to the problems at hand through various technologies that are available,” she said, using e-prescriptions as one clear example of success.
But Hossack doesn’t quite answer how precisely some of best parts of this dynamic will be preserved?
That the panel couldn’t pin down the actual mechanism by which the dynamic could be preserved may simply be because the moderator was asking the wrong question.
It might not be in how the collaborative dynamic created by COVID between government and the sector is preserved. It might be something more simple and tangible set in place which will act as a catalyst for major ongoing change.
It might be the decision to fund a form of universal telehealth.
If telehealth isn’t funded past the end of September in some reasonably universal ongoing form, then the chances of everything going back to the way it was increase exponentially.
How might the change of introducing a form of well managed and regulated universal telehealth catalyse ongoing major innovation or even transformation through the system?
Here are some ideas:
- Every doctor is using it and will continue to use it if it is well managed, providing a central point of technology around which all sorts of fundamental changes to communication and system efficiency can be hubbed. Things like:
- More video consultation, which we know is even more effective for certain patient interactions than telephone alone
- More ability for the system to manage and move to outcomes based consultations rather than time based consultations – presuming that telehealth will seriously challenge the norms of payment via face to face consultation
- More cloud based patient management systems where doctors can be more mobile and more agile in their communications with patients
- A single common point of technology around which other useful connecting technologies will be able to aggregate.
- More data on consultations – both from a patient perspective and doctor perspective
- Hospitals and primary care can be more contiguous in service. Hospital outpatient management can move to telehealth and if need be eventually virtual health assessment, and both primary and allied health could tap into that line.
- Virtual health for all sectors of the community. One huge shift that COVID has prompted is the use of wearables for a lot more out of hospital virtual care.
- A myriad of remote patient management applications for rural care, most importantly perhaps mental health
- A range of applications for allied health professionals to improve the system downstream
- And so on…you don’t have to be that imaginative
The Wild Health panel’s view on telehealth may have been summed up by Grahame Greive’s 22 year old daughter who, in reference to the new telehealth regime and having had her first telehealth consult, said to her father recently with genuine enthusiasm, “isn’t it great that doctors have entered the age of the telephone dad”.
McMahon thinks that we are likely just starting to realise the enormous impact the simple act of allowing doctors to use a telephone can have on the system, pointing out that it will lay a foundation for everything from pre-consultation patient data collection, through an online booking, to a the virtual consult, electronic prescribing and structured patient follow up.
“Having a way for telehealth to be offered in the same way as face to face is a really big turning point,” she told the panel.
“It’s the opportunity for all of us in working in this area to move beyond that linear approach [to innovation]. [It’s the] automation of an existing consultation through to a proper transformation, which would be virtual care. “
Professor Dorota Gertig, Medical Director of Population Health Solutions at Telstra Health, said that her group, which is the largest digital health company in the country, has seen a huge uptick interest from healthcare organisations for the delivery of virtual care as a result of COVID and that telehealth is a base platform around which a more sophisticated virtual care network can be developed across the country.
“From a vendor perspective, it’s been a hugely collaborative time [where people have] really come together to expedite solutions and tailor these to a new way of delivering healthcare,” said Gertig.
“We’re certainly seeing an increased demand in virtual health monitoring so that clinicians can actually connect with patients and monitor their health and well being remotely and not just as a consultation.
“I’m also excited about the possibilities of digital health in health promotion and prevention, I think many aspects of which could be delivered by telehealth.”
Gertig told the panel that she felt that beyond telehealth COVID had emphasised a need for a much clearer national digital infrastructure around infectious disease monitoring and control.
“Multiple call centers, high volume a messaging and sharing data across borders have been key challenges.
“I think this really underscores the urgent need for national digital infrastructure that supports the pandemic response , communicable disease management, interoperability and allows the sharing of data.”
If you want to see the full Webinar you can register and see it HERE
Tomorrow’s live Webinar is Global Trends in Patient Data Management and Alarm Fatigue. REGISTER HERE


