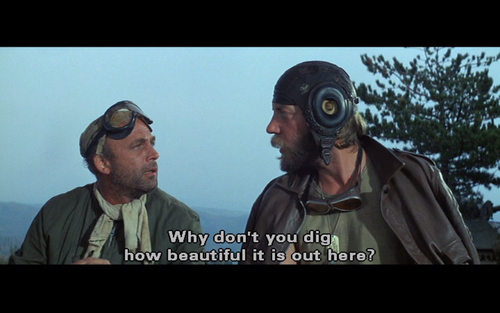
In the Second World War movie spoof, Kelly’s Heroes, tank commander (and hippie) Sergeant Oddball constantly berates his pessimistic private with the line, “Knock it off with them negative waves, Moriarty”. (Moriarty is always pointing out obstacles to the success of the team’s plan).
Ultimately, it’s a movie about motivation and leadership. Oddball’s misfit tank team change the course of the war by leading a charge through enemy lines when no one else can manage to break though.
They are motivated and well led, and their motivation is to rob a bank in a nearby French village.
I’m going to go all “Moriarty” here – at least to start.
Every GP wants to win the war on chronic care and be part of creating a better experience for their patients.
But they aren’t really going to be able to do that while they are threatened with going broke on so many fronts, none of which are being addressed as core goals of the Medicare taskforce.
No amount of saying “Look at the good things we all want to achieve here” and “We’re all in this together” is going to help.
GPs, of all the specialisations, are already the most community-minded.
But if you’re on a slow but sure path to going broke, you’re ultimately not going to engage in much else but trying not to go broke, and worry.
No hard goal to fix GP income or security
Following are the goals of the Strengthening Medicare Taskforce. They are all admirable goals and surely generate a lot of warm and “positive waves”, even within the GP community. They’re hard to be critical of, right?
- improving patient access to general practice, including after hours
- improving patient access to GP-led multidisciplinary team care, including nursing and allied health
- making primary care more affordable for patients
- improving prevention and management of ongoing and chronic conditions
- reducing pressure on hospitals
None of these goals can be achieved if you have a demotivated, disintermediated and broken workforce which is meant to deliver them.
It’s straight-up Maslow’s hierarchy stuff.
If you can’t house or feed yourself properly, you’re hardly going to engage meaningfully in any of the admirable goals listed above.
You’re going to be increasingly distracted by a need to just survive.
Without fixing GP income first and foremost, everything in the taskforce is effectively off the table even before you start.
Some of the things facing community GPs that aren’t being contemplated by this taskforce include:
- A massive shift in payroll and income tax focus by the state and federal tax bodies – created by new tax audit-enabling technologies – which most GP practices aren’t ready for and something that isn’t going away.
- The rise and rise of privately-funded disruptors of community care, such as Pilot, Mosh, Medinet, My Emergency Doctor and many others, which are harvesting low-hanging consultation fruit from largely defenceless small-to-medium GP practices (especially in rural and remote areas) which are unable to organise in the manner of these well-funded commercial ventures.
- A big shift in the focus of many hospitals and LHDs towards following their patients back out into the community and managing them more directly via virtual care, which slices more patient population away from established community-based GP practices. Notably, many of these hospitals would like to work with local GP networks but find it difficult because GPs use old technology that doesn’t connect easily with hospitals, while the current funding paradigm makes it hard for hospitals to use community GP networks.
- The rapid shift in commercial focus by all the large private health insurers to providing community-based care services, often ultimately via contracts with federally funded agencies or organisations, which also eat into the normal patient cohort of a community practice.
- GP corporates, many of whom are now owned by private equity, are organising via technology and efficiencies of scale to grow well beyond their current estimated 25% share of community GP services.
- And there’s more…
The thing is, the world is changing, and community general practice can’t keep up because it’s structurally not set up to be able to move with the times, including how it’s funded – it’s largely a difficult-to-herd mass of small business owners.
An election thought bubble with an unworkable premise
Another billion dollars – promised in the election as a part of the taskforce over three years – isn’t going to fix GP income or strengthen Medicare. In any case, Medicare doesn’t need strengthening, it needs changing.
It’s not even going to come close to helping, especially given some of the already proposed ways we might spend that money.
Infrastructure grants to upgrade practices and new PIP incentives (likely not well controlled or governed) are just two proposed ways to distribute the limited money on offer, both of which sit comfortably within our existing and outdated paradigm for funding primary care.
Given the size of the election win by Labor, and its mandate in winning, it’s in no way politically feasible for this new federal government to spend the sort of money on general practice needed to fix GP income rapidly.
The taskforce billion is token money at best and is being used as a distraction, even if the new government doesn’t realise they are doing that.
“Negative waves, Moriarty… at least the government has committed to one billion. It’s a start. Let’s see what happens here. Get on the new goodwill train and let’s see where it takes us?”
No, let’s not waste more time pretending we are going to make a difference, when the obvious political and economic settings say we can’t do it the way we have promised we might during an election.
Let’s be more honest about the problem and step back and think far more carefully about the nature of problem we have and if there is any way to help general practice within the context of much-needed, whole-system reform.
Let’s look at the whole healthcare system and the fact that we would have a fantastic system – if we were still in the 1960s and still needed to address ill health as our main problem.
Let’s look at:
- The state versus federal funding divide that keeps hospitals and primary care firmly separated from each other when they shouldn’t be.
- Why we fund hospitals and LHDs so much more than primary care when we are all aware that prevention via better connected care in the community is where we need to shift focus and funding.
- A sensible, whole of system roadmap with a proper timeline so as not to threaten just about everyone in the current system, because everyone’s livelihoods and income are tied to a now out-of-date, national healthcare delivery paradigm.
And then let’s see if, within that roadmap, whether we can actually address the issues of income and security properly for general practice in the long term, and provide some form of framework that the GP community of today can work with. And that students who are contemplating become a GP might start feeling more secure about.
Bottom line here: given our system settings, you can’t fix general practice if you’re going to try to do it in isolation from broader system reform.
The usual suspects trying to change a paradigm in which they live comfortably
Does anyone really think that putting most of the same people in the room that were there for the Primary Healthcare 10-Year Plan, albeit this time with some committed election money, is going to change anything for the better substantively?
OK, the new government does need some form of briefing here.
But why are we taking six months to get up to speed?
What is everyone in that room going to say that they didn’t say during the 10-Year Plan discussions? If they start saying things that are wildly different, that’s going to be awkward, surely?
It all feels like politics.
And it’s all a bit too comfortable, given the impending nature of this crisis.
But look, we got everyone in a room, listened, and we’re going to spend some actual money this time.
Who in that room do we think is going to stand up and say, “We’re missing the point entirely by meeting just about primary care; the system is all connected and we all know the system is no longer fit for purpose. We need to step back, and look at the bigger picture and then come back to this”?
The taskforce is largely a group of lobby groups, each with a vested interest in divvying up what little money is now on the table.
It’s not that any of these vested interest parties don’t want to fix the healthcare system. It’s just that within the terms of reference of this particular taskforce, and given its structure, they can’t contribute meaningfully to that goal, so they won’t.
GP income and security can only be addressed in a whole-of-system reform plan
The ugly truth about this taskforce is that it can’t succeed for some very simple reasons:
- It’s not addressing GP income and security as a core starting issue to get its objectives achieved.
- Even if it did decide to address this core issue, it can’t address it in isolation from whole-system reform because there isn’t enough political backing, nor money in the budget, to do it.
We are going to waste time and money here.
We have a giant problem well beyond the breakdown of our general practice community in the short term.
No one is stepping back and asking how we are actually going to properly start shifting our no longer fit-for-purpose monster of a healthcare system towards outcomes-based care.
Only when or if we do that, will we be potentially able to tackle the huge, emerging GP problem we have.
It’s going to be a lot of work. We will likely need a 10-year roadmap and a consistent and well-governed framework because we are talking about altering the course of a massive self-propelling beast.
Unfortunately, it’s not likely that a single rogue tank command is going to be the spark for such a change.
It’s going to require acknowledgement of the broader problem – strange, because it’s so bloody obvious – some courage, and then leadership at the very top to facilitate the mechanisms that would lead to much needed long-term change.
If you’re Moriarty, sitting on your tank on the wrong side of the river, looking at a bombed-out bridge and thinking of the battalion of Germans waiting for you if you do get to the other side, “there’s no way we can do it”. Right?
Wild Health’s Melbourne summit on October 18 will touch on many of the issues raised in this article. If you’re interested, you can see the full agenda and speaker list here and register to attend here. Note: we are starting to run out of seats.

