
This story is coming to you from tropical Prince Charles beach on Taveuni Island Fiji, which although the third largest Fiji Island, is pretty remote (1h and 20 minutes a very small plane from Nadi) and pretty small.
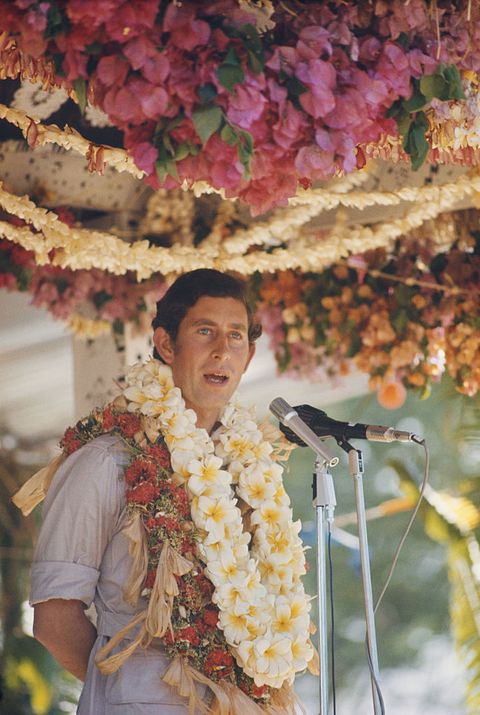
Here is the beach (taken from the bar on the point this morning, where I spend most sunsets drinking Fiji Bitter; the view from where I’m actually writing (a house on the beach at the southern end); and the young Prince (oops King) in Fiji.


I’m now wondering if the name of this beach changes automatically with Charles’ succession.
We don’t have real electricity here yet and run on a generator, which constantly breaks down and is a bit of an environmental disaster.
A few years back the Chinese government, as a part of Belt and Road, built a hydro station down the road. But when the local government stopped getting on with the Chinese, the rollout of the poles and wires stopped, so we have a shiny new mini hydro station on the island, but no wires to get the electricity anywhere.
That’s Fiji … you’ll get it, you just have to wait a bit.
I’m thinking that might apply to a bit to GPs’ thinking on how to get to a better future.
It’s coming (I think).
King Charles did actually visit this beach in 1970 and local administrators immediately renamed the beach after him, which I’m going to suggest might still be one for cancel culture in the coming years as this place is steeped in local tradition and culture.
Its actual name is Vacala Bay, pronounced Vathala.
There’s a couple of reasons to mention where I’m writing from.
The first is tangentially relevant to today’s topic in that it relates to the speed and agility of emerging technology in affecting how flexibly and differently people can do essentially the same job they have for years and potentially enjoy themselves more.
But I mostly want to mention it to one-up a successful ex-employee of mine.
This ex-employee, who we will call Tim, went off and started a successful media business about advertising and media many years ago called Mumbrella, which near destroyed the media and advertising unit we ran, then sold it a couple of years back for a tidy sum, and then, started a new media business (Unmade), but this time from remote Sisters beach in Tasmania.
Every Saturday he writes an op ed, and when he isn’t travelling he always opens up by saying something like (this is an actual opening):
“Welcome to Best of the Week, written this morning at a drizzly Sisters Beach, Tasmania. I’m feeling even happier than usual to be home. During yesterday afternoon’s flight across from Melbourne our pilot informed us that a storm meant our tiny Dash 8 would likely divert to Devonport. That would have left us on the wrong side of the River Cam, where floodwaters yesterday reduced the main Bass Highway to one Lane across the bridge…”
Tim will always then go on to tell you the soundtrack he is writing to, and quote a quirky and often fake world day, before getting to the important stuff.
“Anyway, happy Reptile Awareness day (I think this one is real). I lack the cognitive capacity to curate my own playlist, so today’s writing soundtrack is ABC classic.” (He usually plays Bruce Springsteen).
For all Tim has been successful and at the forefront of using changing technology to build his media businesses, today I win.
Prince (King?) Charles Beach is sooooo much more remote than Sisters beach, it’s golden and sunny (not mostly cold and drizzly), the water is warm, my soundtrack is the Pacific Ocean and the wind rustling through the palm trees, and his “tiny Dash 8”? I flew in on this thing (a de Havilland DHC-6 Twin Otter – 19 seats) into an airport that looks like a rural bus stop.

Still, Tim is happily, and I think successfully, building a new media business from somewhere in small town and remote northern Tasmania, which is something that even 8 years ago, when we started Wild Health’s sister publication The Medical Republic, would have been next to impossible. (Tim didn’t leave TMR, he left the much more clunky Reed Elsevier)
His world has changed radically through technology which he’s embraced. He still does what he loves but he’s doing it where he loves and likely doing it better even. I think he’s happier too.
Could that be a future for GPs if they manage technology well enough in the coming years?
TMR’s world has changed radically as well.
In fact, I doubt that TMR would exist if technology hadn’t offered us so much flexibility and cost efficiency at the outset of us starting up. We could not have afforded to take on the monolith of Australian Doctor and various other long-established players without the utility of cloud and all its business and media apps.
Even back when we started, nearly eight years ago, we could put nearly all our business and functionality on the cloud – accounting and finance, production, email systems, event registration systems … the lot.
I remember being flabbergasted at the time at just how much you could do and how flexible you could be competing with the big guys, with so little. And how much profit we initially made from two derelict divisions we had bought from the big old company (ironically one of them was that media division) for next to nothing because they made no profit.
That big company (Reed Business Information, which owned Australian Doctor at the time) carried a lot of legacy technology that was hard to get rid of overnight, which is a theme that should sound familiar to many GPs.
The sort of change we went though then, and are still going through now, is the sort that a lot of businesses have navigated in the past decade. Banking, travel, media and more have all radically changed.
But not so much general practice.
In fact, not so much medicine full stop.
Medicine has been the great holdout sector as far as digital transformation is concerned.
It has unique qualities – high life and death risk to watch out for, lots of regulation and governance as a result, complex data sharing issues, a lot of government oversight and mostly government based funding – that has allowed it for years to resist technologies like the cloud.
In some instances the tension between the new digital cloud-based technologies and the older server-based ones has created more dysfunction as people struggle to bridge the two systems.
In one respect this has been good for general practice.
The speed and sort of technology changes that occurred in other markets were characterised by significant disruption to a lot of existing businesses.
First movers on new technology often ousted the older established players and the human collateral damage has sometimes been pretty nasty. I’m pretty sure News Corp newspapers have less than one third of the staff they had 10 years ago.
To give you some sense of how fast and how big changes were in some major industry sectors, Tesla, which has been a thing for only 19 years now, has a market capitalisation of over $1 trillion, more than six times the market capitalisation of Ford, which has been going since 1903.
And we all know about the four horseman of the digital apocalypse: Amazon, Google, Apple and Microsoft.
We haven’t seen these dimensions of change in medicine or general practice yet, but we will, and there’s quite a bit of evidence emerging to suggest we are going to see it pretty soon.
Barriers are breaking down in medicine. Big tech is making moves into the sector – Amazon in particular, but all the rest have designs on it. We haven’t got long to figure things out and do a bit of planning.
An Epic battle
A very big thing happened in Australia last week, but if you’re in general practice, it wouldn’t be on your radar, and it would be hard to understand the significance of the event for GPs. But it’s big for everyone in the sector.
NSW Health, which has the largest contract for Cerner (one of the two biggest global hospital EMR vendors in the world) in the southern hemisphere, which means nearly all their hospitals run on its monolithic EMR, awarded their contract for their new statewide single digital patient record (SDPR) to the arch enemy of Cerner, Epic (the other of the two biggest global EMR vendors).
If negotiations stay on track in terms of contractual terms and the funding is found, Epic’s contract will reportedly replace nine existing EMR platforms, six PAS, five pathology LIMS and several other clinical support systems. Although the majority of the existing EMR infrastructure sites are with Cerner, some sit with Orion Health, PAS systems DXC and Citadel, and Lab LIMs with Integrated Software Solutions.
It’s a little confusing at the moment just how much Epic is meant to eventually replace as its not clear in the tender documents and its been hard to pin Health NSW down. Not withstanding, it’s about as big as you can get in terms of a technology contract to underpin a new and more interoperable future for the tertiary side of healthcare in our biggest state.
It will impact GPs in time in a big way. Hopefully a good way.
Until about five years ago Epic had followed a strategy of being a stand alone Epic first and only if possible vendor , preferring not to connect to or talk to any other vendor where possible, but build whole ecosystems comprising all Epic components They did this in the US right down to their hospital EMR implementations talking to general practice and allied health Epic instances of patient management systems.
But in this contract, Epic is going to need to interoperate in many ways with its former arch enemy, Cerner (and some other big system vendors) as this is the EMR in most NSW hospitals currently, and probably will be for some time yet.
Epic sharing data seamlessly with other big vendors like Cerner and DXC is feasible now because in the US, the government mandated some five years ago that every software vendor in medicine needed to be able to put in technology that allowed them to seamlessly share data with each other, and patients who were clients of medical services using that technology.
The initiative was mostly about patient access to data and breaking down vendor strategies to hoard data for commercial gain.
It took five years for US vendors and hospitals to get up to speed on this, but they did.
It means, nominally, Epic can talk to Cerner, which, even a few years ago, was anathema to both companies.
Most of these big hospital platforms can now talk reasonably seamlessly to GP based platforms like eClinical Works and Athena in the US, which are the equivalent of our Best Practice and Medical Director.
Both vendor systems have cloud interfaces they can deploy that make it much easier for them to talk to software vendors outside of their instances in hospitals.
In Australia, this is a little more problematic than the US, because so far the government has resisted mandating data sharing standards and technology, so while the big global EMR vendors have systems with interfaces to do such sharing, nearly every GP patient management system in Australia is still running on very old server technology which is not able to talk back.
The Department of Health is making noises about mandating sharing standards, which would force local big patient management system vendors Best Practice and Medical Director, to move faster to offer software that could easily talk to these other systems.
Medical Director has a cloud version called Helix, but virtually no one uses it, so it’s not really been tested in terms of hospital interoperability. The only other cloud patient management vendor for GPs is MediRecords, and like Helix, it has virtually no share of GP practices (it works a lot with emerging providers of virtual care and governments who are embracing virtual technology far faster than general practice, to make its money).
Best Practice has been contemplating the change to a cloud version for a few years now and it would be surprising if it didn’t have a plan to move quickly if the government moves to forcing them to be more flexible and interoperable with its product.
The Epic NSW SDPR contract feels like a portent for Australian healthcare in terms of getting significantly more serious about its hospitals talking far more seamlessly to primary care.
To give you a sense how fast this trend might move, Epic is the main EMR system being used in the ACT and just this week it a trail was announced to test how the Epic instances of hospital EMRs can talk to general practices in that territory.
If it works it might be a big step in resolving the issue of hospitals not being able to easily communicate with their local GPs in other regions of Australia, likely starting with NSW.
In the meantime, Best Practice is the major investor in a new technology called Halo Connect, a platform that might allow for a bit more speed to market in getting GPs to talk to systems like Epic while our GP platforms are so legacy bound.
Halo Connect is essentially cloud enabling middleware. Versions of this sort of middleware have popped up all over the US to help various vendor systems connect to each other under the new laws on health data sharing there. The more vendors build interfaces to talk to other vendors, the more complex things get, and these middleware vendors step in to help with connection.
To start with Halo Connect will work to connect any cloud enabled interface on an application or platform to the older desktop version of Best Practice via what is called a FHIR interface (which stands for Fast Healthcare Interoperability Resource – essentially a converter to help share health data securely over the web).
Initially Halo Connect is going to allow all sorts of applications which sit on the server version of Best Practice, such as appointment booking systems and directories, to connect via the cloud, which will vastly improve the efficiency of data sharing for BP, the app vendor, and patients who use BP.
But the idea is to expand the platform to connect all sorts of vendors and service providers to each other. Eventually that is potentially going to include hospitals, allied health and even aged care platforms.
Epic in Australia is already in four hospitals in Melbourne, and it has just been implemented in the ACT.
Although Epic’s past has been to hoard data and make it as inaccessible as possible to make it hard for other vendors to work with the company, the US government has done much in mandating sharing standards to break down this issue.
Epic’s NSW SDPR win and an aligned win for them on lab systems in NSW Health alongside it means it will in time dominate the hospital landscape in country (Queensland is Cerner but much of the rest of the country is moving away from Cerner with NSW awarding this contract).
Epic going to need to talk seamlessly to our GP patient management systems soon. Perhaps that’s in part what the ACT trial is about.
In the meantime, in the US, Amazon has followed up on its acquisition of One Medical, one of the biggest virtual general practice service providers to the country, with the establishment this week of Amazon Care, the tagline for which is: “Skip the waiting room and start a virtual primary care or urgent visit from the comfort of your home.”
We wrote about the possible implications of One Medical, and subsequently received a whole lot of mail to the tune of “can’t happen here”.
The only problem with most of that mail is that no one could explain specifically why it won’t, other than the whole idea felt “unAustralian” to some people writing in.
The hint that it could and will happen is the enormous amount of VC and private health insurance investment that is going into virtual GP clinics in Australia.
Eucalyptus, which started with the men’s health site Pilot (now including mental health consults … good grief), and has spread its wings into women’s health and even selling sex toys via a site they are trying to push as sexual health, has been funded in the last year by VCs to the tune of more than $80 million.
NIB has acquired a majority shareholding in virtual provider Midnight Health valuing that group at $48 million and Medibank has invested more than $10m virtual provider MediNet after acquiring a significant shareholding a year ago in MyHealth, a GP corporate.
If these changes aren’t enough to start signalling to anyone that a GP’s life is going to get affected in some way, then start Googling virtual health and in particular pharmacy services.
One of our investors, Tonic Media Network, has even started its own new health economy service called Chemist2U, in which a patient can ask their GP at the time of prescribing to get their prescription sent directly to their home at the click of an app, so they don’t have to bother picking it up.
The app talks directly to the major patient management systems and is hooked to pharmacies in most regions in the country. It’s gaining a lot of momentum as a business.
Key immediate changes GPs are going to need to embrace are the rise and rise of the virtual providers and, perhaps more usefully, the rise of connectivity to the greater health economy, in particular to hospitals, which are all needing to work much more closely with GPs to manage their patients far better out of hospital.
Although most people groan at the prospect of Amazon starting Amazon Care in Australia, it’s quite possible that such a situation might improve the lot of some GPs by providing well paid and flexible new job opportunities (I’m not a fan of this theory).
In all of it this there is both threat and opportunity.
As I wrote last week, I’m the last person to understand what GPs are thinking and why, but in all of this it feels like with the right amount of openness to change, and perhaps taking the odd calculated risk or two, GPs could navigate in a manner that my ex employee Tim has done in the last 10 years – make the technology work for them in a big way.
But that’s not going to happen if the big players don’t step back and think about what is happening and how they can engage with it.
This isn’t being done, openly at least, by the AMA and the RACGP. Both are tending to work to the old model of GP care and trying to maintain it, rather than talk to GPs about navigating some of the inevitable change that is coming.
It’s a lot about technology, but probably a lot more about culture.
At its heart GP culture is about community care: about understanding their patients better than anyone through a longitudinal care relationship and making more informed decisions about that care as a result. It’s also traditionally been a culture of the resilient.
It should be some comfort to know that it doesn’t feel like all these changes will substantively change any of that culture wise.
But at the same time, it doesn’t feel like the standard bricks and mortar, somewhat disconnected care model that most practices run on today will be easily maintainable.
Some things will need to change.
Embracing interoperable technology, working with hospitals much more closely (and probably aged care), and forming virtual co-ops to build your own virtual care services to compete with the VCs and private insurers will all need to happen.
And it can.
What else might happen with this is the ability to further embrace one of the great aspects of GP culture: the ability to work part time, the ability to work and be a mum, or a dad who’s more of a carer, or do other tangential things that bring you a little more variety and joy in your working life.
Almost all GPs are frustrated creatives. The new technology feels like it’s going to help future GPs embrace their creative selves. Creative Careers in Medicine (CCIM) run by the entrepreneurial GP Dr Amandeep Hansra is successful and growing because GPs want more variety in their working lives, and increasingly, this is possible.
There’s a lot of doom and gloom out there in GP land created by the inability of government to keep patient rebates indexed properly to the cost of living in a stressed system, by technology in state offices catching up and forcing practices to re-engineer their accounting to avoid payroll tax stings, and by the encroachment of tech companies whose culture is fast profit not community care, in the virtual space.
But there is plenty of room for GPs to flex their operational priorities and status in the coming of open systems technologies. In fact, there’s room in there for relatively small set ups to start organising against the set ups with a lot of capital, even the big corporates.
All in all, there are plenty of reasons to remain optimistic.
And plenty of things about the profession – its variety, its flexibility, its community focus – to start rebranding and attracting new students too.
Technology and culture are key.
Technology is changing seismically.
Culture will need to adapt to the changes, but essentially, resilience and a strong focus on care of the community is going to remain at the core.
That’s it from me for a bit.
I’m going for a quick surf (there’s a small wave just below the sunset bar on the point with no one else ever on it as we are too far away from everyone – what joy).
After that I’ve got to get out some EDMs, pay some suppliers, set up a new rego page for a new event next year, and write another story for our digital health channel.
All in time to catch the late afternoon sunset at the bar with a Fiji Bitter.
Now wondering if I can’t just stay here for a couple of months.
Declaration of Interests:
- Tonic Health Media Network owns 10% of The Medical Republic
- The author is a non executive (and unpaid) director of MediRecords
GP transformation Summit 2023
If any of the topics in this story have been of interest to you, you might be interested in participating, contributing or helping with a new GP summit The Medical Republic is organising for mid-September next year which will deal with changes to the GP profession under the themes of Technology, Business and Culture. The summit will feature leading thinkers on all aspects of how GP lives are changing and include practical hands on ways to prepare for and engage with change. Some of the topics covered will include:
- the digital future of managing your personal tax and payroll tax for contractors and owners
- building your own virtual practice
- when and how to move to the cloud in your practice
- how your patient management vendor can help your transition
- contractor versus owner versus start up
- connectivity to allied health and aged care
- leadership for effective change in disruptive times
- Australia’s most likely health reform roadmap and timetable and how GPs fit into it
- optimising part-time work
- realising your creative urges.
If you’re interested in helping and have some ideas you can email jeremy@medicalrepublic.com.au or michelle@wildhealth.net.au.

