23 September 2021
The emerging potential of “balancing system load” with virtual services

Telehealth and smart virtual services that are starting to aggregate around it offer us significant new opportunities to manage healthcare budgets more efficiently, while maintaining and sometimes even improving access and safety.
Large electricity stations are the most capital intensive investments for state governments and up to four times the cost of large new city based hospitals, so it’s not surprising that the economics of electricity generation has some firmly established fundamentals which enshrine a lot of efficiency in resource allocation and sharing.
The most fundamental concept in affording electricity generation (until now – things are changing because of coal) is base load versus peak load supply integration, something that deals with the biggest system issue in generation, a substantive 24 hour cycle of peaks and troughs in demand.
Big, usually coal fired, base load power stations handle about 80% of all generation at a very low relative cost per kilowatt generated, but running them for that final 20% to meet the peak loads which only last for 2-3 hours at a time during a day is vastly expensive. So, we have smaller agile peak load stations (often gas, now more and more renewables) which fire up quickly during the day to deal with these peaks.
With Australia embracing telehealth at scale by deciding to rebate it on the MBS, we’ve introduced to our healthcare system something of the potential of the economics of load balancing in power generation.
MBS rebated telehealth, and the many smart web and mobile enabled consumer access services that are starting to form around its core, are presenting opportunities for the system to ‘balance its system load’ far more efficiently than it has ever done before.
The examples of where this is starting to occur are many, and most are in their still in their infancy. They include simple GP telehealth in cases where the opportunity cost for a patient and doctor to make a physical appointment has a bad ROI for both them and the system, hospital in the home services, aged care in the home, rehabilitation service post hospital care such as cardiac and wound care rehab, and of course all manner of remote and regional services.
One emerging service which seems like a bit of a no brainer in this opportunity is My Emergency Doctor (MED), although it should be noted that MED does not currently get any MBS funding.
At its heart MED is just a bank of on-call emergency specialist doctors (all 90 or so are Fellows of the Australasian College for Emergency Medicine, FACEM) who are made available virtually for any circumstance in the system where our base load capacity for the emergency care expertise on offer is being exceeded, and we need an efficient means of meeting peak demand.
Given the nature of emergencies is that they are mostly unexpected events, planning for emergency lends itself naturally to a base and peak load model.
While most of our rural and remote state run hospital groupings have for obvious reasons usually set up versions of virtual support to manage the far more problematic supply and demand problem for emergency medicine in the country, you can imagine that there are always times when there is a peak on a peak, and a rural hospital or region is found short.
Rarely will you find an emergency specialist on staff at 3am in a regional hospital, and even though there will often be one on call, providing some support and back up after 11pm at night for those on call goes a long way to increasing the overall wellbeing and efficiency of those consultants that are on call.
MED offers a sort of failsafe option for any LHD, LHN, or HHS wanting insurance on such situations.
It also offers the ability for the state health departments to manage gaps that might naturally emerge in their system from time to time due to all manner of labour supply issues in the regions.
Perhaps unsurprisingly, MED has found that it is not a bad thing that big city hospitals are finding the ability to have a relief valve on tap in their EDs.
It has recently secured contracts with some Victorian hospitals, and one NSW hospital, to take the load off their big city hospital emergency staff on the low priority end of their workload – the triage category 4 and 5 patients – for those situations (an asthma storm perhaps) which require all hands on deck for far more serious peak emergency load incidents.
MED also has contracts with a few PHNs to fill in that gap in a system where after hours calls need an emergency physician to make a better determination of whether someone needs to push the button on getting an ambulance, and sending someone to hospital or not.
Given the cost issues of when someone arrives via ambulance and they don’t actually need to, there is obviously a lot of cost and labour efficiency to be had if the MED service can more effectively make these calls. Such efficiency gains flow both to a PHN and the related hospital group in any region.
As with a lot in digital health, it feels like it has taken a pandemic to make the sort of utility of a service like MED become a lot more obvious.
That and the availability these days of cloud based technologies which allow the group to use FACEMS in all time zones for the sort of flexibility you need to operate past 3am. The groups tech stack includes cloud patient management system MediRecords for clinical notes and collation and Twilio to co-ordinate voice calls, videos calls and SMS as essentially a purpose built cloud based multi-channel call centre.
In the last 18 months, the service has grown enormously. Some hospitals have contracts with the service as cover for managing base load stress which is being induced by covid, especially in circumstances where some hospitals lost workforce to isolation requirements.
More assistance to patients who are being managed in the home is a another key area where the service is helping.
But its FACEMs are called on to lighten the load in the hospital ED department itself by helping sift through the triage 4 and 5s, leaving the onsite staff the time to deal better with the urgent load.
“The business really is about providing our healthcare system complementary access to emergency specialists, for those times, and places when that access is most difficult,” says CEO of MED Bill Maiden.
“We are a partnering provider of care when frankly, the system struggles to be able to cope with unforeseen and sometimes consistent spikes in demand.”
The mother of all unforeseen and consistent spikes in demand started some 18 months ago, coincidentally, when Maiden took over the role of CEO from FACEM founder Dr Justin Bowra. Dr Bowra started the group in 2016 and built it steadily over the intervening years via capital raises, to being some 90 FACEMs strong.
Dr Bowra, who is the groups Medical Director, continues to be a strong champion of telehealth and tele-education, advocating long before covid pushed MBS rebated telehealth firmly onto centre stage in our arsenal of tactics to manage the crisis.
In some respects MED was purpose built to help in a crisis like covid, and as a result the growth of business in the last 18 months has been huge, as it has taken on contracts to assist EDs in NSW and Victoria, and to assist with some of the management of covid patients at home. He predicts that, based on contracts just secured, the group is going to grow over the next couple of months by over 30% alone.
So far the group has not done much work in Queensland but Maiden says the infrastructure and capacity of the group is now there to be able to help out in that state as well a lot more, if administrators see the need.
Maiden believes that beyond covid (and of course as a result of it largely), MED and similar virtual services like it, are destined to be more recognised now for what they can achieve in the system because they’ve proven so useful in battling the crisis.
But he still acknowledges that virtual services are a balancing act between supply, demand and the very real remaining need for expert feet on the ground – the base load – especially in rural areas.
According to Dr Angus Ritchie, one temptation for health bureaucrats with labour issues in the regions might be to replace labour problems with virtual where on the ground resources remain a vital part of effective care.
Dr Ritchie runs one of the country’s most interesting hospital in the home trials out of RPA hospital in Sydney, and is strong proponent of virtual technology support as an extension to hospital services. Covid has seen that trial expand into helping handle large stresses in the in system in parts of Sydney during lockdown.
He says that too much reliance on telehealth and virtual technologies in the regions, as useful as they are, could end up denuding the quality of care if on ground expertise, which is expensive but vital to quality of service, gets replaced for economic reasons.
Not withstanding, any debate over the utility of telehealth and associated virtual technologies, especially with respect to funding, is all but over.
Given its proven effectiveness in delivering system efficiency when applied in the right way, it’s hard to see the government rescinding MBS for telehealth, although surely budget issues will force some modification of the current covid settings for rebates.
In this respect, services like MED look like they have an important role to play moving forward in a system that in a post covid budget constrained environment will need more than ever to seek the balanced line between efficiency and safety of care delivery and cost.
Says Maiden, “At the end of the day, it’s just about access to a doctor when you need it. If that’s your problem, then we can find a myriad ways to deliver that to you in a way that works best for a group in need. That’s the problem we solve.”
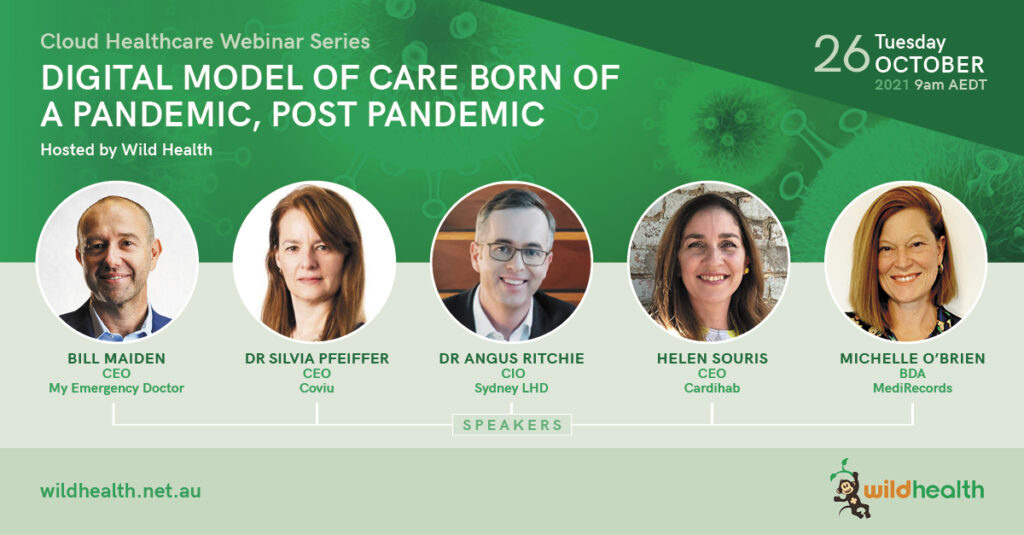
If you are interested in new models of care, Wild Health is hosting a series of webinars looking at this topic and others relating to cloud infrastructure in Australia. Read more and register here.