Wild Health Canberra Australian health leaders’ summit
Tackling our biggest barriers to starting long-term healthcare reform
In a pre-budget check-up of the Australian health system, Wild Health is going to Canberra on 4 May 2023 to examine how we might navigate the most intractable barriers to our starting meaningful, long-term healthcare reform.
The past three years have challenged our healthcare system. But they have also delivered us opportunities, with examples of how it is possible to change the way we do things, at scale and rapidly, showing us how we could potentially reform and strengthen healthcare.
Wild Health Canberra will bring together key health leaders and influencers from across the country to take part in an interactive series of short talks, panels, interviews, and mini workshops in an attempt to build consensus on how we can overcome the significant barriers to beginning reform
Key themes of the summit program will include:
· Working with a federated system of governments to build effective, integrated regional care organisations
· Building a national 10-year set of objectives with all stakeholders
· Strategic assessments on a regional basis
· A roadmap for aligning funding and technology settings to meet the objectives
· Whether the development of clinical and ethical standards for healthcare, along with standards for technology and data sharing, can help
· Understanding the nature of an outcomes-based system before moving towards it
· Interoperability as a catalyst for delivering equity
Wednesday 3 May: Pre-Summit events (SOLD OUT)

12:15pm – 1:45pm
Lunchtime Panel
Join us the day before the summit for a sit down lunch. The panel discusses modern and efficient healthcare systems, the role of new and emerging models of care to alleviate pressure on our hospital system, and also the role of Public/Private partnerships in the future of health.
Panelists:
- Hans Erik Henriksen, Past CEO, Healthcare Denmark
- Professor Zoe Wainer, Deputy Secretary, Public Health, Victorian Department of Health
- Toby Hall, Past CEO, St Vincent’s Hospital
- Ian Galvin, CEO, Ramsay Connect
- Matthew Galetto, CEO, MediRecords
Moderator: Jeremy Knibbs, publisher at The Medical Republic and Wild Health

2:00pm – 5:00pm
Pre-Summit Health Reform Workshop
Moderated by Jay Rebbeck (Rebbeck), Kylie Woolcock (AHHA) and Tim Blake (Semantic Consulting)
Strawman: The desired 10 year position of the five key elements of our healthcare system
- International co-commissioning expert Jay Rebbeck will engage a room of key leaders in the the now, feasible near term, and desired 10 year state of the key elements to our healthcare system.
- The workshop will look at lateral ideas such as a possible mechanism for state and federal oversight and cooperation in funding and policy execution, a significantly expanded co-commissioning ecosystem, aligning technology and standards for data sharing within and between the regions and bringing patients on the journey.
The workshop will bring together healthcare leaders from PHNs, hospitals, aged care, allied health and technology innovation.
Findings of the workshop group will be presented in the summit on May 4.

5:00pm – 7:00pm
Networking Drinks
A two-hour cocktail reception for workshop participants.
Thursday 4 May: Main Summit, 8:30am – 4:30pm
REGISTRATION: 8:30am

8:50am – 9:05am
Looking across the valley of health reform despair
Everyone either talks or writes about health reform. Everyone has a view on what we need to do. Sometimes, some well meaning insiders even start the odd pilot. But nothing much happens. There are currently huge barriers to shifting a system that has been so successful for so long, that is tied to a federated model of government funding, and which involves so many component parts that don’t talk to each other. So we stand on one side of the valley of health reform despair, pining for change but not knowing how to begin to cross the valley. This summit is about strategies and tactics to get started on the journey. It will look at:
- A sick care system not a health care system built more than 50 years ago
- Funding models that don’t take into account the future of outcomes-focused care
- A workforce under severe stress
- Inefficient ways of working and perverse funding models that duplicate services and management
- The lack of policy directives on interoperability
- Siloed, disconnected technology across the sectors
- Planning for 10 years and working backwards
- Aligning component parts of the system without centralised or co-ordinated leadership
- Identifying and aligning the component parts of the system that are moving towards reform but still need help
- Co-ordinating a coalition of the parties that are willing to traverse the valley
9:05am – 9:25am
Jeremy Knibbs in conversation with Dr Stephen Duckett
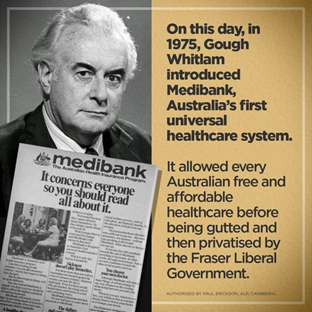
What would Gough Whitlam make of our universal healthcare system now? Can we reinvigorate the fading dream of universal healthcare?
And if we can, where do we start?

9:25am – 10:10am
Panel: Is this the health system Australia wants in 10 years’ time?
With the vision of universal healthcare and health equity in ruins, everyone seems to have a quick band-aid solution to healthcare access. From pharmacists prescribing and state-run urgent care clinics to virtual emergency departments and hospitals employing GPs to run end-to-end integrated health hubs for those who can no longer afford to see their GP.
Even private health insurance wants a role in the delivery of primary care.
Ironically, patients are now more confused and frustrated than ever about where to go for care.
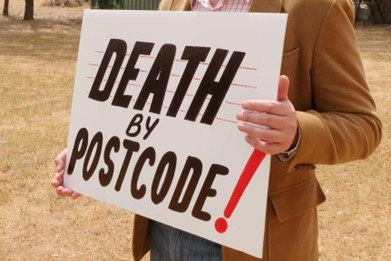
With bulk billing disappearing and a shortage in the health workforce now critical, the vision of cradle-to-grave healthcare, with continuity of care provided by a GP, is dimming fast.
Are we in danger of returning to pre-Medicare days, when healthcare was a luxury available to those who could afford it, while those who couldn’t just accepted second best?
Panelists:
- Dr Michael Bonning, President, AMA NSW
- Ray Messom, CEO, WentWest
- Dr Rob Grenfell, Chief Strategy and Regions Officer, Grampians Health
- Scott Willis, National President, Australian Physiotherapy Association
- Clare Mullen, Deputy Director, Health Consumers’ Council WA
Moderator: Jeremy Knibbs, publisher at The Medical Republic and Wild Health
Topics:
- How do we start better navigating the politics of state versus federal funding that often leads to the duplication of services and perverse funding models?
- How do we flip the system to make it more consumer-focused?
- Our hospitals are adopting virtual and value-based care models and extending their reach out into the community to capture patients who are ageing or have poorly managed chronic disease but who are still slipping through the cracks.
- Our underfunded primary care practices are struggling to survive and can no longer offer bulk billing, pushing patients to look for more affordable alternatives.
Healthcare reform is urgently needed to save what was once a world-leading health system.

10:10am – 10:55am
Presenting the findings of the pre-summit workshop
The workshop’s objective was to provide a framework for building a 10-year plan on which all stakeholders can collaborate.
The panel will review the basics of process and change management in complex systems, and look at what is required to catalyse effective, long-term change, including identifying the basic components of a 10-year plan.
Panellists:
- Neil Deacon, Partner, Rebbeck
- Tracey Johnson, CEO and Company Secretary, Inala Primary Care
- Kylie Woolcock, CEO at AHHA
- Dr Paresh Dawda, Director and Principal, Prestantia Health and Next Practice Canberra
- Tim Blake, Managing Director of Semantic Consulting
Moderator: Jay Rebbeck, Managing Director, Rebbeck Consulting
Topics:
- Do we really understand the problems?: A strategic assessment framework
- Could we achieve state and federal collaboration in an integrated regional management model?
- Modelling needs and requirements for iterative funding steps
- Managing political conflict during the process
- Governance
- Starting at the end: What are the obvious objectives everyone can agree on?
- Working backwards:
- What are the challenges if we introduce those objectives too quickly?
- Are there easily identifiable “stepping stones”?
- Audience and panel strawmen for moving to a roadmap:
- The real potential of co-commissioning

10:55am – 11:15am
Morning Tea
11:15am – 11:55am
Panel: Changing rural and remote management to a single management structure faster
Panellists:
- Andrew Coe, CEO, Western NSW Primary Health Network
- Ben Chiarella, Head of Innovation, Ramsay Connect
- Dr Hamish Meldrum, Owner and Director, Ochre Health Group
- Bronwyn Phillips, Manager Remote Patient Monitoring, Bendigo Health
Moderator: Dr Rob Grenfell, Chief Strategy and Regions Officer, Grampians Health
Topics:
- Rural and remote is vastly different from urban. Can, and should we draw a line?
- Should we have different funding models to meet the needs of rural communities?
- Rural and remote is already in crisis, with few GPs and massive challenges in doctor recruitment and retention. Doesn’t a single regional integrated group make more sense?
- Western NSW has launched a partnership between the NSW Rural Doctors Network, Western NSW LHD, the Far West LHD, and Western NSW PHN to combat diabetes, with funding from the NSW Government.
- What is the role of co-commissioning in this context?
- How do we bring together the collective wisdom and lessons from every pilot to create a national resource?

11:55am – 12:00pm
Sponsor Spot
Ben McEvoy, CTO, Evrima

12:00pm – 12:20pm
20 minutes with Dr Nicole Higgins, President of the RACGP

12:20pm – 1:10pm
Panel: Tackling the biggest untalked about obstacle of all: How the public perceives healthcare delivery and spending
Panellists:
- Clare Mullen, Deputy Director, Health Consumers’ Council WA
- Dr Emily Kirkpatrick, Executive Medical Director, Calvary-Medibank Joint Venture
- Ray Messom, CEO, WentWest
- Elizabeth Koff, Managing Director, Telstra Health
- Bronwyn Morris-Donovan, CEO, Allied Health Professions Australia
Moderator: Jeremy Knibbs, publisher at The Medical Republic and Wild Health
Topics:
- The big, shiny hospital dilemma: How do you educate the public about priorities in an outcomes-based system?
- How does our healthcare system work for the consumer?
- The political dimension: Pharmacy prescribing and big hospitals win votes. Or do they?
- The practical question of public perception and how we change it.
- From patient and consumer voice to public perception and voting power.

1:10pm – 1:50pm
Lunch
Afternoon Sessions

1:50pm – 2:10pm
How ready is Australia to deliver health and social care in the home?
Jeremy Knibbs in conversation with Hans Erik Henriksen, Toby Hall and Sarah Barter for a discussion about how Denmark used reform to shift care into the home and the challenges and opportunities for Australia to support our ageing population to stay in their homes.
From July 2024 there will be a new program that provides in-home care services for older Australians. This new program is called the Support at Home Program and it will replace the current Commonwealth Home Support Programme (CHSP), Home Care Packages (HCP) Program and the Short Term Restorative Care (STRC) Programme.

2:10pm – 2:50pm
Panel: How effective will healthcare reform be without an interoperability strategy to underpin it?
Reforms that move the healthcare system towards value-based care will need real-time data that flows with the patient between providers.
Models of multidisciplinary team care can only deliver outcomes if they are able to access the data to support informed decisions.
Technology has an important role to play in driving innovation that will help deliver value-based care, protect program sustainability and support the health workforce.
Panellists:
- David Rowlands, Managing Director, Digital Health Leadership Australasia
- Grahame Grieve, Health Intersections, Founder FHIR
- Ben McEvoy, Chief Technical Officer, Evrima
- Andrew Aho, Regional Director – Data Platforms, InterSystems
- Matthew Galetto, CEO of MediRecords
Moderator: Tim Blake, Managing Director, Semantic Consulting
Topics:
- How is the lack of interoperability impacting health equity in Australia and how do we change things?
- How can data sharing enabled by interoperability support a move towards value-based care?
- Why we need a policy directive for standards, like the US 21st Century Cures Act, to remove silos and attract investment in innovations.
- Are Australians missing out on life-changing innovations because we are falling behind?
- Who is responsible for building the framework to support innovative technologies here?

2:50pm – 3:00pm
What does the data say about Australia’s readiness for Digital Transformation?
Tim Blake (Managing Director, Semantic Consulting) shares some fascinating and surprising insights into how Primary Care is adopting and using Digital technology across Australia.

3:00pm – 3:15pm
Building a sustainable nursing and midwifery workforce
Karen Booth (President, Australian Primary Health Care Nurses Association) and Alison McMillan (Chief Nursing and Midwifery Officer) in conversation with Jeremy Knibbs about the long term challenges for these vital professions.

3:15pm – 3:25pm
Afternoon Tea

3:25pm – 3:40pm
15 minutes with David Dahm, CEO and Founder, Health and Life
What would a set of peer-reviewed sustainable clinical and ethical standards in medicine and healthcare professions do for reform and the healthcare industry globally and locally?

3:40 pm – 4:30 pm
Panel: How do we retain and improve access and equity in a reforming system?
Panelists:
- Jane Bollen, Primary Healthcare Nurse Consultant
- Dr Walid Jammal, GP, Hills Family General Practice
- Dr Mike Millard, Clinical Director, Clinical Research Unit for Anxiety and Depression
- Leanne Wells, Director, 89 Degrees East
- Scott Willis, National President, Australian Physiotherapy Association
Moderator: Tracey Johnson, CEO and Company Secretary, Inala Primary Care
Topics:
- How do we address inequity in health and social care?
- How do we put the spotlight on funding prevention and early intervention to stop people getting sick?
- How do we include social determinants such as poverty or digital inequity as part of a holistic approach that allows us to identify those most at risk of chronic illness or mental health problems?
- How do we create the framework and funding to use digital tools and GP social prescribing strategies to prevent the progression of chronic conditions and to lessen the impacts of ageing diseases and polypharmacy?

4:30pm – 5:30pm
Networking Drinks
That’s a wrap!
Registration Enquiries:
conferences@virtuallyassisted.com.au
Program, Content and Panelist Enquiries:
Michelle O’Brien
Partnership Opportunity Enquiries:
John Todd

Professor Enrico Coiera
Director, Centre for Health Informatics, Australian Institute of Health Innovation

Professor Farah Magrabi
Professor of Biomedical and Health Informatics, Australian Institute of Health Innovation

Daniel McCabe
First Assistant Secretary - Medicare Benefits and Digital Health, Australian Government Department of Health, Disability and Ageing

Dr Suzanne Miller
Director of Strategy, Quality, and Technology / Clinical Deputy Director, Victorian Virtual Emergency Department

Associate Professor Amith Shetty
Clinical Director System Sustainability and Performance, NSW Ministry of Health